Since their discovery, antibiotics have been prescribed against bacterial infections of all kinds. Whether it’s an annoying earache or a full-blown pneumonia, antibiotics got you covered.
But you might wonder what precisely these “miracle drugs” are. And how do they function? What sort should you take, and where can you find them? We will answer all of your questions and provide you with all the information you want. Let’s begin!
1. What Are Antibiotics?

They’re not like common painkillers or allergy medications. Instead, antibiotics are tailored to target bacteria. Their mechanism of action can differ; they either eradicate bacteria entirely or halt their multiplication.
Alexander Fleming’s pioneering work cannot be overlooked here.
Why? In 1928, he discovered the first antibiotic—penicillin. And this discovery changed how we viewed diseases. Back then, an infection could take your life. But suddenly, we had a way to fight deadly infections that we once thought were untreatable.
2. Are Antibiotics Easily Accessible?
Antibiotics are not available over the counter. In most places, you need a prescription from a healthcare professional to obtain antibiotics. This requirement is in place to ensure that antibiotics are used appropriately and only when necessary. Using antibiotics without a prescription can be dangerous and contribute to the problem of antibiotic resistance.
If you’ve been prescribed antibiotics and are wondering what pharmacies offer free antibiotics, check out Lakeview Pharmacy. They provide free antibiotics to all customers through their free antibiotics program. Get in touch with them to learn more.
3. How Do Antibiotics Work?
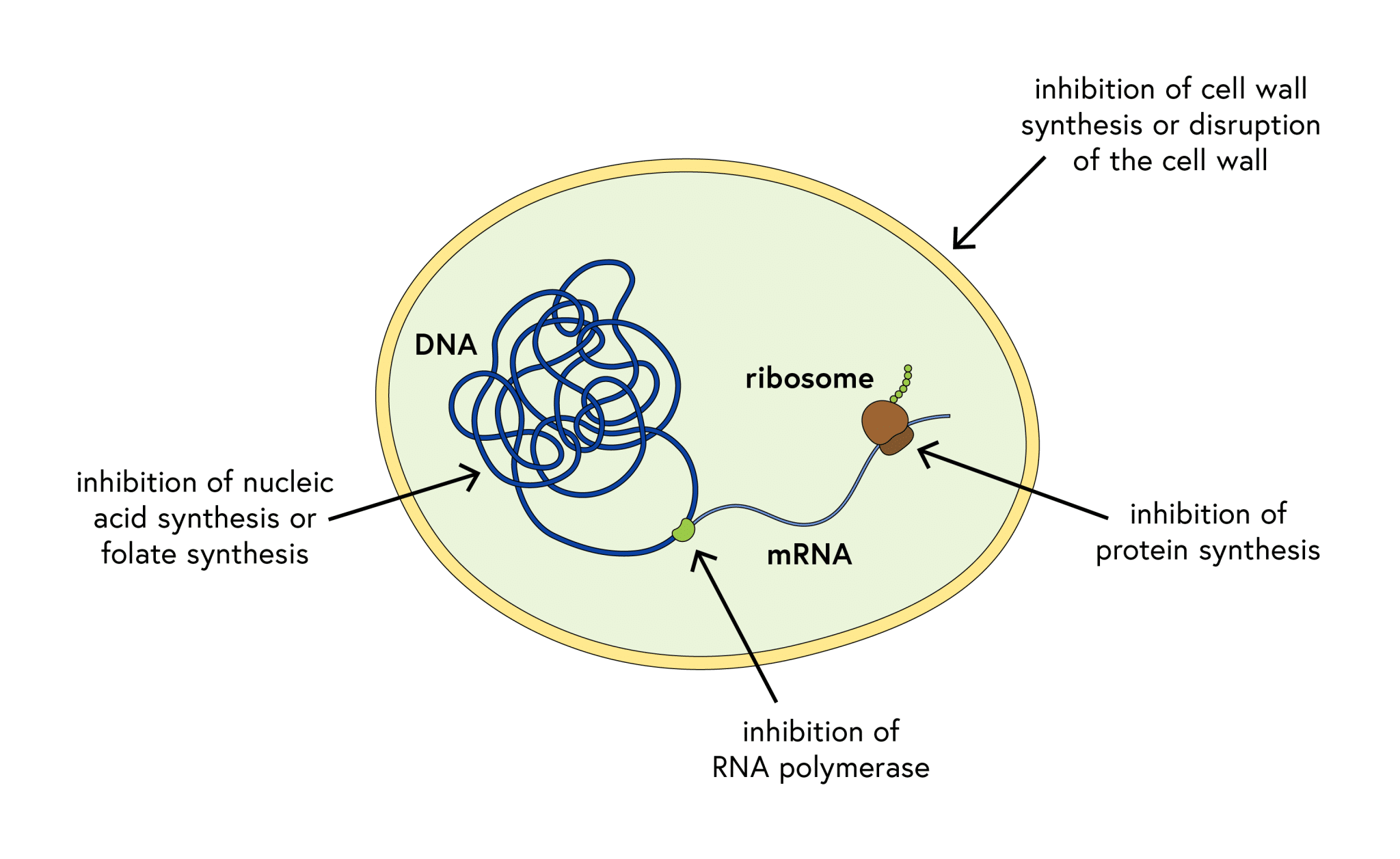
First, we have the “bactericidal” antibiotics. These are responsible for killing harmful bacteria. They attack the bacteria’s cell walls or disrupt their internal workings, effectively eliminating them.
Then there are the “bacteriostatic” antibiotics. These take a more subtle approach. They don’t kill the bacteria outright, but they slow down their growth and reproduction. This gives your immune system a helping hand and they come in and mop up the remaining bacteria.
4. Types of Antibiotics
Over the past century, scientists have continuously researched and created many different types of antibiotics. Some of the prominent ones:
- Penicillins: This family includes the well-known amoxicillin. It is one of the most commonly used antibiotics. Their effectiveness against various bacteria makes them a great choice for various infections.
- Cephalosporins: These antibiotics, with ceftriaxone as a prime example, are often reserved for more serious infections. They work in a similar manner to penicillins, but they are effective against a wider range of bacteria.
- Tetracyclines: This group, encompassing drugs like doxycycline, is versatile. It tackles infections ranging from acne to respiratory ailments.
- Macrolides: A popular member of this drug class is Azithromycin. It is the solution for individuals allergic to penicillin. It proves effective against skin and respiratory infections.
5. When Should You Take Antibiotics?
Antibiotics are, in fact, our main line of defense against infections. But let’s not forget that they don’t always work. And only a licensed doctor can determine whether they are necessary or not. Why? Because they particularly target and eliminate bacteria. They might not be effective against viruses like the flu or the common cold.
Some common conditions where antibiotics may be prescribed include:
- Bacterial pneumonia
- Strep throat
- Urinary tract infections
- Skin infections
But before you take antibiotics for any of these conditions, it is important to consult a medical professional.
This is because misusing antibiotics can have serious consequences. One way to misuse antibiotics is by taking them for viral illnesses or not completing the full prescribed course. It not only renders the treatment ineffective but also contributes to the growing problem of antibiotic resistance.
6. How to Take Antibiotics Correctly
The wisest thing you can do when taking antibiotics is to take them according to your doctor’s instructions. Your doctor will give you specific instructions on how to take the medication.
This usually means taking your pills at the same time every day. And here’s the thing: even if you start feeling better before you finish all the medicine, that does not mean you can stop taking the medicine. You might want to stop taking your meds once you get better, but that isn’t such a good idea.
It can leave some of those nasty bacteria alive, making them stronger and more resistant to these antibiotics.
7. Side Effects of Antibiotics

Some of the more frequently reported side effects include nausea, diarrhea, and stomach discomfort. These arise because antibiotics, in their pursuit of harmful bacteria, can inadvertently disrupt the beneficial bacteria residing in our gut.
In some individuals, antibiotics may trigger allergic responses. These reactions can manifest as mild skin rashes or escalate to severe, life-threatening conditions such as anaphylaxis. If you have a history of allergies or experience any adverse reactions while taking antibiotics, it’s imperative to communicate this with your physician. They can then modify your treatment plan or recommend ways to alleviate the side effects.
8. Antibiotic Resistance
The rising tide of antibiotic resistance poses a significant threat to our health. This phenomenon occurs when bacteria, in a display of adaptability, evolve mechanisms to overcome the very drugs intended to eradicate them. Consequently, infections become increasingly difficult to treat, escalating the risk of disease transmission, severe illness, and even mortality.
One of the primary drivers of this worrisome trend is the misuse and overuse of antibiotics. Instances such as taking these medications unnecessarily, failing to complete the full prescribed course, or using them inappropriately can inadvertently foster resistance among bacteria.
To counter this growing issue, it’s important to take antibiotics responsibly. This entails taking antibiotics only when deemed necessary by a healthcare professional and adhering strictly to their instructions.
Conclusion
Antibiotics are a powerful tool in fighting bacterial infections, but their effectiveness depends on their correct use. Understanding what antibiotics are, how they work, and when to take them can help ensure they remain effective for future generations.
It’s also crucial to be aware of the dangers of antibiotic resistance and to take steps to prevent it by using antibiotics responsibly. While natural alternatives can support health, they should not replace prescribed antibiotics for serious infections. Follow proper medical advice and stay informed about antibiotics.

